Case of 42 y old male with CKD on MHD and orbital cellulitis?
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings investigations and come up with diagnosis and treatment plan.
Name: P.Nikitha
Roll no: 102
A 42 year old male , resident of Choutupal Who is daily wage labourer by occupation came to opd for regular dialysis.
History of presenting illness:
Patient was apparantly asymptomatic 1 1/2 yr back
Then after taking covid vaccination he developed fever
Fever was present through out the day
Not associated with vomitings,nausea,burning micturition .
Generalised weakness was present
Didnt relieve on taking medication also
So he visited our hospital.
Then he was diagnosed with hypertension and renal cyst. For which he was given medication.
After 6 months he developed shortness of breath and pedal edema upto ankle for a week. Then they visited Gandhi hospital
Where dialysis was done for him and was admitted in hospital for nearly 20 days
And then medication was given.
2 months back he developed shortness of breath and generalised weakness again
Now he visited our hospital. His hemoglobin levels are low so blood transfusion of 4 units was done .since then he was on regular dialysis which is twice in a week.
15 days back after dialysis was done
He developed watering eye in the right eye,peri orbital swelling was developed,tenderness was present,no eryyhema
And then gradually vision was lost in that eye with in 5 days.
After 7 days he noticed nasal bleeding from right nostril. He also develped an ulcer like
Wound on his right nadolabial fold of nose.He also developed a swelling on the scalp on right side for which he was treated with fudic ointment.
Past history
Known case of hypertension since 1 year and on medication
Initially 1 year back he used to take 1 tablet /day now he is using 3 tablets / day
Not a known case of diabetes,TB,asthma
Personal history
Mixed diet
Appetite is reduced
Normal bowel and bladder movements
Sleep is adequate
Addictions
Chronic alcoholic
Daily consumption of alcohol around 250 mL for around 20-25 yrs and stopped 1 1/2 yr back
Daily routine
Before 6 months
He used to wake up at 5:00am and does some house hold works and goes to work at 8:00 am after having breakfast and returns home at 3:00 pm for lunch and goes back to work and again returns home back between 8-9pm and will have dinner and sleep
Now
He wakes up around 7:00 am and after taking shower will have breakfast by 8:00 am and then sleeps again and wakes up at 2:00 pm for lunch takes his medications and sleeps again and wakes up again at 8 pm will have dinner and sleeps again.
Family history:
Not significant
General examination
Patient was conscious ,coherent and well oriented to time and place.
Patient was moderately built and nourished
Vitals
Blood pressure : 160/100 mm Hg
Respiratory rate: 17 cycles /min
Pulse: 80 beats/min
Temperature: 99 F
Pallor is present
No icterus,cyanosis,clubbing,lymphadenopathy
Local examination
Eye:
Right eye
Mild swelling of upper lid is present
Conjunctiva is muddy
Cornea is clear
Loss of vision is present
There Is no counting fingers ,perception of light
Ocular movements are limited in all
Directions
Direct and indirect Light reflex are absent
On palpation mild tenderness is seen
Nose
Epistaxis from right nostril
Mild tenderness is present in maxillary region.
Ulcer like wound is present om the right nasolabial fold of nose.
Head:
Single follicular cyst was seen on right side in frontal region
Which was relieving with medication
Systemic examination:
CVS- S1 S2 heard no murmurs
CNS- No focal neurological deficit
RS- Normal vesicular sounds heard
Provisional diagnosis:
Chronic kidney disease on maintenance hemodailysis
hypertension since 1 1/2 yr
With periorbital cellulitis?
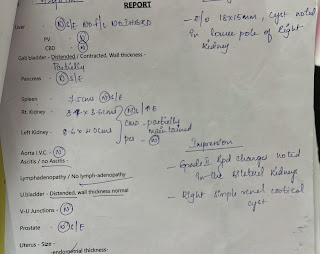
Investigations:
Treatment:
Fluid restriction <2L /day
Salt restriction<2g/day
Tab Nicardin 10mg po /Bd
Tab shelcal 500mg po/Bd
Tab Nodosm 500mg po/Bd
Tab Oroferxpo po/oD
Tab bioD3 weekly once
Inj Angmatin 600mg iv/TLD
Inj.clindamycin 600mgiv/TLD
Case discussion from PaJR group
[6/20, 8:38 PM] Can the vesicles be due to herpes zoster?
Can loss of vision be due to hypertensive retinopathy or due to increase in IOP?
[6/20, 9:59 PM] : Herpes zoster opthalmicus?
[6/20, 9:59 PM]Which positive findings made you suspect it?
[6/21, 8:02 AM] Rakesh Biswas sir :Share a scientific journal case report link of a patient who had herpes Zoster ophthalmicus with findings similar to your patient, quoting the relevant portions from that link
[6/21, 8:09 AM] 2018 KIMS Ug: A herpes zoster ophthalmicus rash involving the tip of the nose (alae nasae) is known as a positive Hutchinson's sign. This indicates nasociliary nerve involvement; the nasociliary also innervates the eye.
https://casereports.bmj.com/content/2014/bcr-2014-204566
[6/21, 8:10 AM] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4692814/. Herpes zoster ophthalmicus occurs when the latent varicella zoster virus (VZV) reactivates in the trigeminal ganglion and ophthalmic branch of the trigeminal nerve. In the elderly, there is a sharp increase in the tendency of secondary skin bacterial infections occurrence due to the deterioration of capabilities of self-care and changed sanitation. We present a case of patient who developed phlegmon of the orbit, which resulted with complete unilateral blindness.
[6/21, 8:34 AM] Rakesh Biswas sir :What is the reason for our patient's loss of vision? Anatomically if the Zoster is confined only to the 5th nerve why should he lose his vision?
[6/21, 8:38 AM] : Herpes zoster can also cause the cornea (the clear layer in front of the iris and pupil) to become swollen, severely damaged, and scarred. When the structures behind the cornea become inflamed the pressure of the fluids inside the eye can increase to the point that it begins to damage the optic nerve. Ultimately this can result in glaucoma, a serious condition which can result in permanent vision loss.
[6/21, 8:42 AM] Rakesh Biswas sir : @Senior Sir Your description of the patient's vision, eyes and CNS findings is inadequate.
[6/21, 8:43 AM] Rakesh Biswas sir :Clarify all these findings in our patient with the ophthalmology today and share their notes
21/06/23, 10:55:35 AM] Nikitha Palnati: Eye findings
Right eye
Eyelid: mild swelling on upper eyelid
Conjunctiva: muddy
Cornea : clear
Pupil: fixed,not reacting to light sir
On fundoscopy
Pale optic disc
[21/06/23, 10:58:09 AM] Rakesh Biswas Sir: What is the vision in his right and left eyes?
[21/06/23, 11:04:51 AM] ~ Manish Kumar: Right eye complete loss of vision ... Left eye vision present sir
[21/06/23, 11:07:43 AM] Rakesh Biswas Sir: No perception of light in right eye?
How much vision in left eye?
[21/06/23, 11:08:53 AM] Rakesh Biswas Sir: Any case report of Zoster ophthalmicus having similar findings @918008996036 ? What is his loss of vision due to?
[21/06/23, 11:12:54 AM] ~ Manish Kumar: Can be due to involvement of nasociliary nerve sir
[21/06/23, 11:55:00 AM] ~ aashishyadlapally: Can it be optic neuritis or retro bulbar neuritis causing loss of vision
[21/06/23, 7:46:03 PM] Nikitha Palnati: Sir
Can it be periorbital cellulitis? Which is leading to eccentric proptosis and which may lead to optic atrophy and causing vision loss ? In this case
[21/06/23, 7:49:21 PM] Rakesh Biswas Sir: How would periorbital cellulitis cause optic atrophy?
21/06/23, 7:52:09 PM] Nikitha Palnati: Proptosis might lead to optic nerve compression?
21/06/23, 7:53:15 PM] Rakesh Biswas Sir: How? Any review of literature. Then all thyrotoxicosis patients would lose their vision?
21/06/23, 8:08:53 PM] Rakesh Biswas Sir: What have we done to help this patient till now? What is the diagnosis for his skin lesions and vision loss?
[21/06/23, 8:22:27 PM] Nikitha Palnati: Skin lesions are intially vesicular and now crusting type sir
We have sent patient for dermatology referral and they suspected it might be due to insect bite or herpes zoster Opthalmicus and they gave an ointment sir after using that lesions have reduced to some extent.
He also had a follicular cyst on scalp for which also he used the same ointment and now it also reduced
Patient was also sent for Opthal referral sir , he has to visit yesterday again but he couldn’t .
We also took a tissue sample from nose and waiting for histopathology reports
[21/06/23, 9:04:33 PM] Rakesh Biswas Sir: What ointment is Fusidic cream and what role does it have?
[21/06/23, 9:16:25 PM] Nikitha Palnati: Sir
It’s an antibiotic
Used to treat bacterial skin infections
[21/06/23, 9:17:28 PM] Nikitha Palnati: Generally used in conditions like infective dermatitis and impetigo sir
[21/06/23, 9:31:36 PM] Rakesh Biswas Sir: So how did it help your patient?
[21/06/23, 9:38:15 PM] Nikitha Palnati: After using that
His itching got reduced sir
And also size of swelling on scalp also reduced
[21/06/23, 9:39:39 PM] Rakesh Biswas Sir: So it's a bacterial infection and not herpes zoster ophthalmicus?
[21/06/23, 9:43:08 PM] Nikitha Palnati: Might be bacterial infection sir
Because his symptoms got reduced
[21/06/23, 9:47:23 PM] Rakesh Biswas Sir: Which bacteria will lead to loss of vision and complete extraocular muscle paralysis?
[21/06/23, 10:02:33 PM] Nikitha Palnati: Sir normally
Bacteria like streptococcus and staphylococcus can cause periorbital cellulitis sir
[21/06/23, 10:02:48 PM] Nikitha Palnati: And periorbital cellulitis can lead to this symptoms
[21/06/23, 10:04:10 PM] Rakesh Biswas Sir: So your current diagnosis is bacterial orbital cellulitis causing optic atrophy and visual loss and not zoster?
[21/06/23, 10:12:03 PM] Nikitha Palnati: The clinical features of orbital cellulitis included proptosis, swelling of the eyelids, conjunctival chemosis, and limited ocular motility.1 There may be exposure keratopathy resulting in corneal ulceration. The vast majority of these patients present with local symptoms such as edema, erythema, pain, chemosis, decreased ocular motility, and proptosis
[21/06/23, 10:13:00 PM] Nikitha Palnati: Specifically, the incidences of decreased visual acuity, proptosis and external ophthalmoplegia are more closely associated to orbital cellulitis.1 Temperature greater than 37.5°C and leukocytosis resulting in fever is a more prominent feature in the pediatric group. External ophthalmoplegia and proptosis may be the most common features, while decreased visual acuity and chemosis may be less frequent in pediatric cases as well as in adults. Involvement of the optic nerve may produce papilledema or neuritis with rapidly progressing atrophy resulting in blindness.
[21/06/23, 10:13:30 PM] Nikitha Palnati: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3277022/
[21/06/23, 10:23:39 PM] Rakesh Biswas Sir: This was very useful to understanding the case. Please share it in the group along with your inputs?
2/06/23, 9:03:32 AM] ~ Dr.Dinesh Datta: So,can it be Mucor causing the lesion on nose and eye?
[22/06/23, 11:28:14 AM] Rakesh Biswas Sir: He would have died by now if it was mucor. We saw quite a few of them during covid here
[24/06/23, 1:56:16 PM] Rakesh Biswas Sir: This same patient seen by 33-48 interns yesterday was transferred to NIMs
[25/06/23, 8:23:02 PM] Rakesh Biswas Sir: Update by our UG :
Good evening sir
I spoke with his son sir
Update is :
He is better than day before yesterday but not yet recovered sir.
Apparently doctors told them that there is infection because of central iv line and they changed its location it seems sir and dailysis was done.
And about eye doctors told them that they will treat that after he recovered from this it seems sir
[10/07/23, 2:39:24 PM] Rakesh Biswas Sir: Patient update?
[10/07/23, 2:40:30 PM] ~ Dr.Narsimha Reddy: The Patient Was Admitted in NIMS & They Thought that Eye Involvement is due to Stroke Sir
[10/07/23, 2:44:01 PM] Rakesh Biswas Sir: Stroke in which anatomic location would cause that?
[10/07/23, 2:48:46 PM] ~ Dr.Narsimha Reddy: PCA Stroke Can Cause Such Symptoms Sir
[10/07/23, 2:51:08 PM] Rakesh Biswas Sir: Explain how
First share his findings and then interpret them
[10/07/23, 4:33:18 PM] ~ Dr.Narsimha Reddy: He was Having Weakness in Left UL & LL along With Restriction of Eye Movements in Right Eye Sir Which Could be Weakness Can Be Explained be Left MCA Territory Stroke Sir
[10/07/23, 4:34:23 PM] ~ Dr.Narsimha Reddy: But Restriction of Eye Movements Can in All Directions Can't be Explained by this Stroke
[10/07/23, 4:36:40 PM] Rakesh Biswas Sir: Then how would you explain it? Can you share his detailed CNS findings at that time?
[10/07/23, 4:37:23 PM] ~ Dr.Narsimha Reddy: On MR Venogram He Was Having Cavernous Sinus Thrombosis Which Could Explain his restriction of Eyemovements Sir.
10/07/23, 9:06:35 PM] Nikitha Palnati: Sir can this be due to the same bacterial infection which lead to orbital cellulitis and he also had maxillary and frontal sinusitis from which it might spread into cavernous sinus and ultimately lead to thrombosis
[10/07/23, 9:08:41 PM] Nikitha Palnati: Optic neuritis and scleritis can be changes occurred post cellulitis ?
[10/07/23, 9:15:06 PgM] Rakesh Biswas Sir: Did our patient have cavernous sinus thrombosis or ica thrombosis?
[10/07/23, 9:24:41 PM] Nikitha Palnati: Sorry sir
[10/07/23, 9:24:50 PM] Nikitha Palnati: Our patient had ica thrombosis
Read this report carefully
[11/07/23, 8:29:47 AM] ~ Dr.Narsimha Reddy: Okay Sir
[11/07/23, 8:35:03 AM] Rakesh Biswas Sir: Share what you understand about the cause after reading it
[11/07/23, 11:00:27 AM] ~ Dr.Narsimha Reddy: Sir Visual Loss Can be Due to to 2 Reasons one can be due to Thrombosis of Cavernous Part of ICA ( As Cerebral Part of Gives Opthalmic Artery ) & the Other Reason could be due to Optic Neuritis ; Restriction of Movements can be Due to Scleritis Sir ??
[11/07/23, 11:04:41 AM] Rakesh Biswas Sir: 👆So you have changed your opinion on this
[11/07/23, 11:25:18 AM] ~ Dr.Narsimha Reddy: Yes Sir ...But In Cavernous Sinus Thrombosis also there can be Ophthalmoplegia
[11/07/23, 12:26:19 PM] Rakesh Biswas Sir: We want to know about our present patient's problem. General knowledge we are expected to have learned in the past
[11/07/23, 12:27:05 PM] Rakesh Biswas Sir: How would ICA thrombosis cause optic neuritis! 😳😨
11/07/23, 1:46:47 PM] ~ Dr.Narsimha Reddy: I did not mean ICA thrombus causes Optic Neuritis Sir
I told visual loss can be caused by these two reasons ( ICA stroke and optic Neuritis)
[11/07/23, 1:58:42 PM] Rakesh Biswas Sir: So how do we explain his optic neuritis?
[11/07/23, 1:59:52 PM] Rakesh Biswas Sir: How does visual loss happen due to ICA obstruction and how do you explain his extraocular muscle paralysis?



























Comments
Post a Comment